Exceeding expectations,
together
Full pathway
Healthshare is the only community provider to offer whole pathway solutions of integrated care. Working in partnership with the NHS, we deliver high quality, efficient, evidence-based care. Through a flexible approach, we can offer stand-alone services or full pathway delivery.
We deliver system wide benefits in terms of cost-effectiveness, improving patient access, quality of care and patient outcomes.

Integrated MSK physiotherapy
Healthshare offers a fully integrated approach for patients with MSK problems, effectively managing 80% of patients in community and primary care settings while providing evidence based, quick routes to imaging and surgery where necessary. By providing every step of the MSK pathway, our services are patient centred, efficient and cost effective.
Full diagnostic suite
We offer complete diagnostic services from X-ray through to cross sectional imaging and endoscopy, improving patient access by providing a variety of sites from primary care to our own Community Diagnostic Hubs and acute hospital sites. Working in partnership with the NHS, we provide fully staffed mobile services, quickly adding diagnostic capacity to local health systems.
Population coverage
7.2 million
people a year
Effectively managing
500,000
patient episodes per year
Recommended by
93%
of patients
Case studies

Community diagnostics centres
Healthshare is building state of the art centres to provide additional diagnostic capacity closer to home.

First contact practitioners
Healthshare’s advanced MSK practitioners work in primary care to help patients get early access to specialist expertise and reduce GP workload.
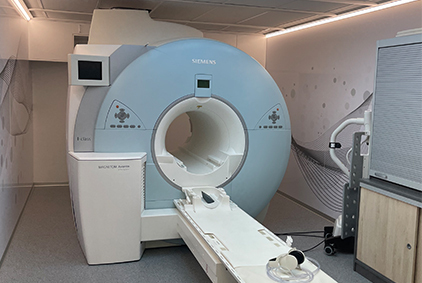
Mobile MRI
Healthshare delivered a mobile MRI solution for an NHS Foundation Trust in 3 weeks, adding diagnostic capacity to support COVID recovery.

Shoulder ‘one stop shop’
By challenging conventional thinking and putting patients first, we have improved health outcomes and increased efficiency of service delivery.

Digital MSK Wellbeing Platform
Healthshare rapidly developed an online Digital MSK Wellbeing Platform that supports patients in their own home whilst they wait for surgery.
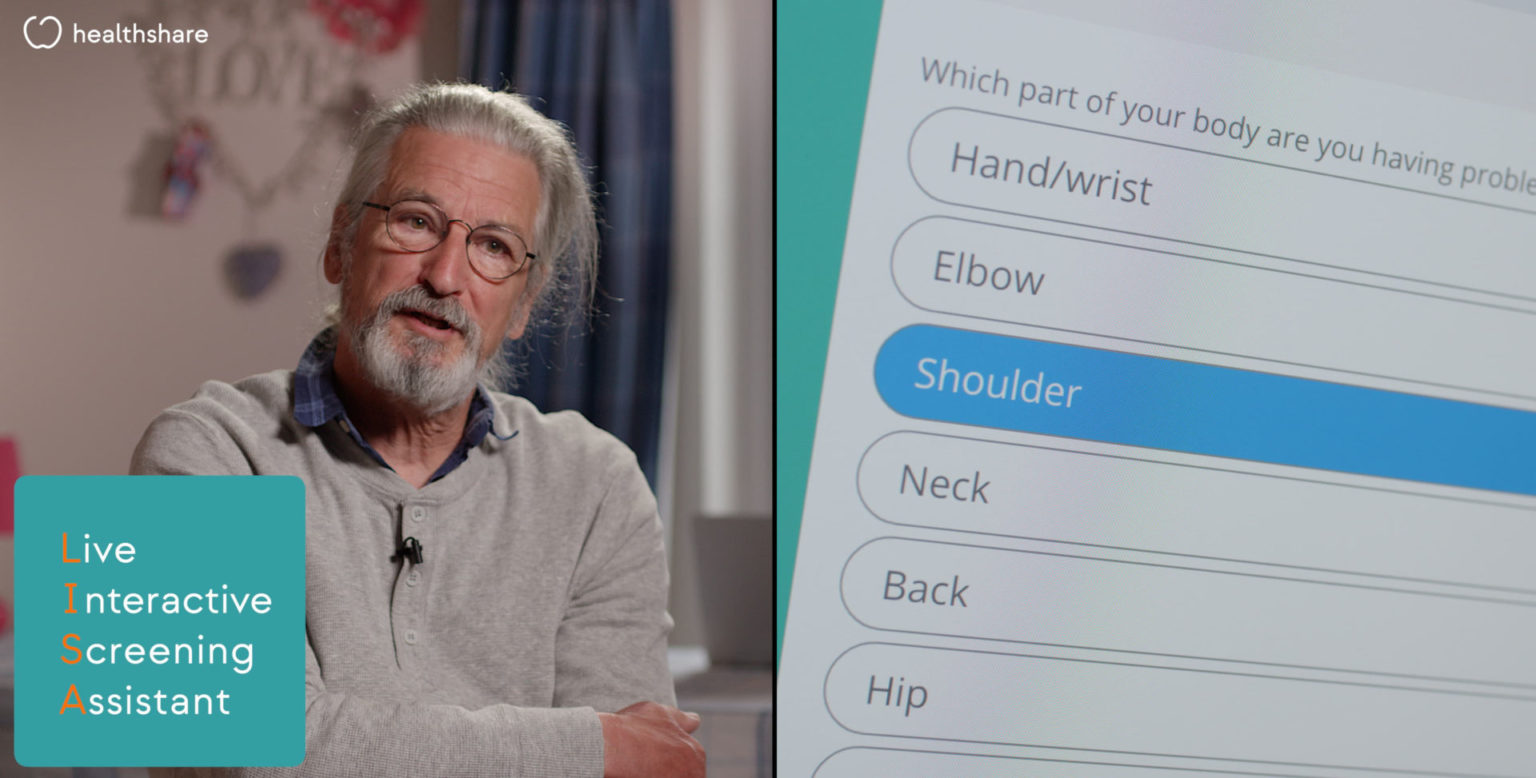
Digital MSK pathway
Healthshare’s Digital Pathway, including the Joint Pain Advisory Clinic and triage with LISA, transform how MSK care is delivered.



